Neurologic manifestations of COVID infection
June 3, 2020
Discovery of effective treatment for COVID-19 Infection
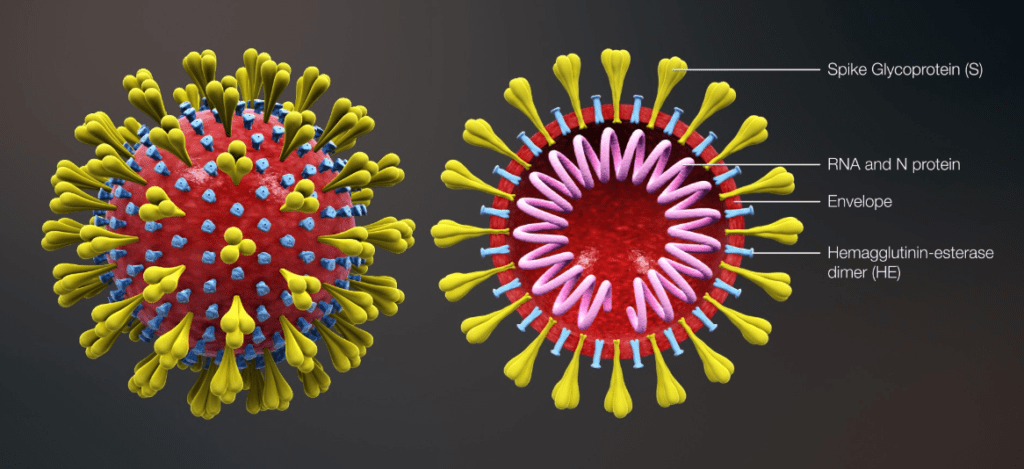
June 16, 2020Corona virus is a single strand, enveloped RNA virus. Corona derived from Latin, meaning crown [viral envelop has crown like projections].It is most likely originated from bats [or may be pangolins].
So far epidemiological data suggests that <0.01% of those infected require hospital treatment, with a majority showing very minor symptoms, or none at all.
Transmission

Transmission is mostly by respiratory droplets. These are larger particles that are released with coughing or sneezing and usually fall to ground or other surfaces within 6feet of the source person.
As air borne transmission can happen health workers working in closed contact with COVID-19 patients should use N-95 masks.
As virus can survive on surfaces for hours contact precautions are of utmost importance, such as wearing gloves at public places, frequent hand washing etc.
Most of the infection spread is likely to occur through infected individuals without symptoms or infected individuals who will eventually develop symptoms (30% to 50%).
One infected person can spread infection to a large number of individuals in crowded conditions.
Corona virus enters cells via ACE-2 receptors which are expressed by inner cells linings of lungs, intestine, Kidneys and blood vessels.
Subsequently, additional damage is caused by specific type of proteins released by affected cells that harm other cells of body [cytokine storm].
SYMPTOMS

Fever, cough, fatigue and shortness of breath are the most frequent symptoms. Other symptoms are anosmia (loss of sense of smell), purulent conjunctivitis (red eye with discharge) and gastrointestinal Symptoms such as diarrhea, vomiting etc.
Myocarditis (inflammation of heart muscle) is an infrequent but serious complication of COVID-19.
It can be associated with pericardial effusion (accumulation of fluid around heart), and patients with myocarditis are at increased risk of death, due to cardiac arrhythmias (irregular heart rhythm).
Most patients (81%) have mild illness.
14% may require hospitalization and 5% could end up in ICU care.
Symptoms alone are not sufficient to distinguish COVID-19 from other respiratory viral infections.
Mortality

Subjects 60 years or older are at increased risk of death, when compared to younger healthier adults.
It also depends upon co-morbid conditions such as underlying cardiovascular diseases, chronic respiratory disease, diabetes and malignancy.
Although, uncommon, young healthy adults can also develop severe illness, could require ICU care and deaths have also been reported.
LABORATORY FINDINGS
Common finding are
- Blood reports can show elevated or low white blood cells counts.
- Elevated liver enzymes.
- Chest x-rays could be abnormal in only half of the patients.
CT scan is more sensitive.
But these imaging findings are not specific for COVID-19.
- Nasopharyngeal swab for SARS-COV-2 PCR seems to be the most appropriate diagnostic test at this time.[detecting presence of virus in infected individual’s secretions].
- Serology could be helpful in estimating prevalence of the disease. As it can show presence of IgG in plasma of individuals who recovered.[ IgG are special proteins called antibodies which our immune system produce to fight infections].
Management
Stable patients breathing comfortably are advised to self-isolate at home. They are advised to use Acetaminophen for fever and myalgia, keep themselves hydrated. If condition worsens contact health officials.
Patients with moderate to severe symptoms should be hospitalized for observation and treatment.
Critical patients may need ICU care.
Antiviral medications are under trial and more data and research is required to prove their efficacy.
Patients recovered from COVID-19 have neutralizing antibodies against the virus. So in theory antibodies from patients recovered should help.
PREVENTION

Taking preventive measures can play crucial role in this pandemic control.
They include
Social distancing
Frequent hand washing
Staying home or self- isolation when sick
Universal masking can prevent infection spread particularly by asymptomatic carriers [30 to 50% of infected individuals] or people having mild infection as this will protect other healthy individuals from being exposed to their respiratory droplets.
Health care should follow their institutional guidelines.
Preventive measures can slow the epidemic termed as, “flattening the curve”, easing the burden on health care system.

https://medium.com/@Riz98/sars-coronavirus-2-2019-a-primer-covid-19-6cc8e48fa58f