How Can Cardiovascular Risk Be Reduced in Kidney Dialysis? How Can Cardiovascular Risk Be Reduced in Kidney Dialysis?
June 5, 2024Why Are We Undertreating So Many Pulmonary Embolisms? Why Are We Undertreating So Many Pulmonary Embolisms?
June 5, 2024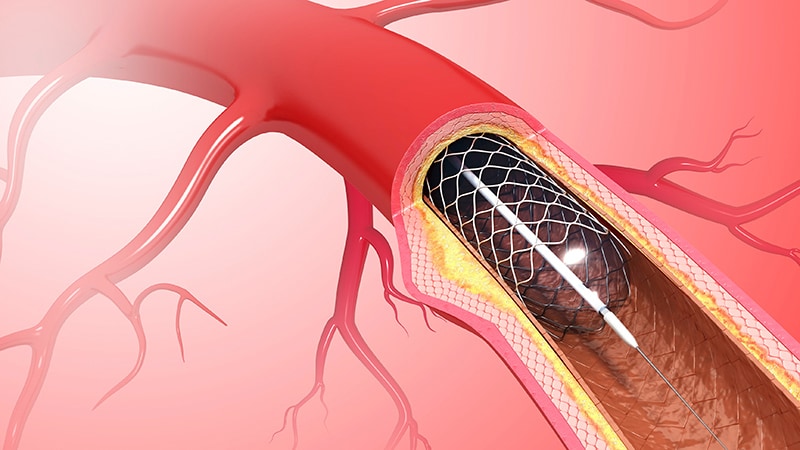
LONG BEACH, California — Percutaneous coronary intervention procedures performed using the radial artery in the arm have almost tripled in the past decade, according to a new study evaluating 6.7 million PCIs from the CathPCI Registry.
Although the approach is superior to femoral artery access on three key cardiovascular endpoints, it carries a slightly higher risk for stroke, which hasn’t appeared in clinical trials, the investigators reported.
“The study demonstrates a sea change in the manner in which PCI is performed in the United States, but also highlights the continued opportunity for practice improvement with dramatic inter-operator variation,” Reza Fazel, MD, a cardiologist at Beth Israel Deaconess Medical Center in Boston and lead author of the study, said during his presentation of the results at the Society for Cardiovascular Angiography and Intervention (SCAI) 2024 Scientific Sessions.
The real-world results, which also show that the highest-risk patients likely derive the most benefit from radial artery access, come from a retrospective cohort study that evaluated temporal trends in transradial PCI and used an instrumental variable analysis to compare the two PCI access routes (in 2.2 million procedures from the same registry performed from 2018 to 2022).
“There’s still a lot of operator-level variation in the use of radial PCI,” Fazel said after his presentation. “This shows there’s a lot of room for improvement. We’ve made progress but we still have a lot to do.”
This study also shows that “there are benefits from radial PCI in terms of reduced mortality, reduced bleeding, and reduced vascular complications that are replicated in the real-world setting, and that the benefit is highest in the highest-risk patients, STEMI [ST-elevation myocardial infarction] patients,” Fazel said.
However, the adjusted event rate for stroke was higher with radial PCI than with femoral catheterization (0.32% vs 0.27%).
A Stroke Signal
“It’s a very small signal, which none of the existing trials have been powered to detect, but this database is big enough that we can see that signal,” Fazel said. “We believe it’s real, and it’s a causal link between radial access and that small increase in stroke.”
During the study period, 40.4% of all procedures were performed using radial access, but the rate rose steadily from 20.3% in 2013 to 57.5% in 2022, which is a 2.8-fold increase.
The risk for death was lower with the radial approach than with femoral access (1.16% vs 1.31%), as was the rate of major access-site bleeding (0.34% vs 0.98%) and the rate of other major vascular complications (0.12% vs 0.32%).
“There are very clear benefits in terms of reduced mortality, reduced major bleeding, and reduced major vascular complications,” Fazel said. “The magnitude of those benefits far outweighs that risk of stroke. It’s important to know it’s there, but the strong recommendation for preferentially using radial access where possible is not changed by that.”
The slightly higher rate of stroke with transradial PCI did not surprise nor faze Ian Gilchrist, MD, professor of medicine at the Penn State Milton S. Hershey Medical Center in Hershey, Pennsylvania.
“The question of whether stroke is a real risk or not has swayed back and forth through multiple studies in the past, and the rate of stroke is so low that it’s very hard to pick it up in small studies or do any kind of randomized studies,” he said.
The mere nature of PCI using the radial artery, which requires moving the catheter past the junction of the carotid artery, creates a slightly high risk for stroke, Gilchrist said. The study may be picking up a technical issue with operators who aren’t as facile with the radial approach as the femoral access. “It’s really unclear,” he said.
“The net result, though, is that I don’t think we should be dissuaded from using the radial artery because we’re worried about the stroke, because that risk is very small,” Gilchrist said.
Benefits With Radial vs Femoral Access
Patients with serious heart disease had an even greater benefit from the radial approach, the analysis showed. For patients with STEMI, the absolute risk difference for death between radial PCI and femoral access was -0.43%, for major access-site bleeding it was -0.89%, for other vascular complications it was -0.18, and for stroke it was 0.09; this surpassed outcomes for patients with non-ST elevation acute coronary syndrome and nonacute coronary syndrome.
Could this be the last word on transradial PCI?
“I don’t know that there’s anything else in this directional path that needs to be clarified,” Fazel said. “There are subgroups that are worth looking into, such as patients with prior bypass surgery; it’s a more tedious process in those patients in terms of the technical burden on the operator,” he pointed out.
“But in terms of this specific question of the superior safety of radial vs femoral, I think we have pretty solid data there and I don’t anticipate any other large trials happening in that area.”
