FDA Delays Approval for Eli Lilly’s Experimental Alzheimer’s Treatment
March 12, 2024After SABR, 100% Local Control at 1 Year in Kidney Cancer After SABR, 100% Local Control at 1 Year in Kidney Cancer
March 12, 2024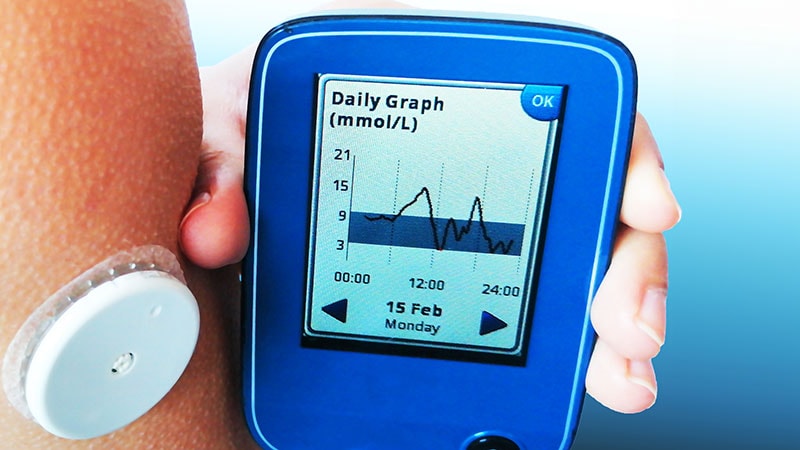
Are you helping your patients with type 1 diabetes make the most of continuous glucose monitoring (CGM) devices? At the Advanced Technologies & Treatments for Diabetes meeting, two leading CGM experts offered “pearls” and “tips” for clinicians.
Cari Berget, RN, CDCES, director of the PANTHER program at the Barbara Davis Center for Diabetes at the University of Colorado Anschutz Medical Campus, presented five general “pearls” for CGM use. Endocrinologist Steven V. Edelman, MD, professor of medicine at the University of California San Diego, delved into the nuts & bolts, with tips beyond CGM use to general helpful advice for managing type 1 diabetes.
Berget based her talk on materials from PANTHER, an educational program developed to translate trial data and clinical practice experience into resources for both clinicians and patients. She noted that CGM is now standard for people with type 1 diabetes and is increasingly showing benefit for people with type 2 diabetes.
Moreover, she noted, “CGM is also the cornerstone for automated insulin delivery (AID). So, it’s important in and of itself as a tool but also as a way to access the most advanced insulin delivery technologies that we know give us the best chances for the best glycemic outcomes.”
These were her five takeaways:
1) Be intentional about equity. This advice arose from several studies showing that CGM use and other diabetes technology is lower among Black vs White patients, even after adjustment for socioeconomic status and type of health insurance.
“What this tells us is there are other factors…that are playing a role. One of those factors might be implicit bias,” she said.
On a positive note, a targeted quality improvement project in Alabama dramatically reduced disparities in CGM prescribing based on race, insurance status, and diabetes characteristics.
The way to address this, Berget advised, is to “implement a standardized approach for recommending technology based on evidence, not subjective beliefs and arbitrary metrics like A1c or number of fingersticks per day.”
2) Focus on skin care. Skin problems can present a major barrier to CGM and insulin pump use. The PANTHER website has an entire section on “skin solutions,” with sub-pages devoted to device placement techniques, skin irritation prevention, advice for keeping the devices stuck on the body, device removal and healing, and a list of helpful products.
3) Personalize alarm settings. These should be based on individual goals and alarm tolerance, Berget advised.
“There are so many alarm options on many of these CGMs, but for a lot of people, more is not better. So just because we have a predictive alarm does not mean we should be using it across the board. Alarms need to have a specific reason for their use that’s perceived as useful by the user. And then it needs to have an action plan associated with it. What are you going to do if you get this alarm? Without these pieces alarms just become burdensome, and they make people want to quit their devices. And they stop responding to those alerts.”
4) Tailor CGM education and incorporate psychosocial supports. “If the perceived benefit of the technology outweighs the perceived burden, that person will continue using the device. So, it’s very important that we understand for each person,” Beget advised.
Areas of focus here include problem-solving in social situations, troubleshooting hassles of device wear, working through concerns related to trusting the device, perceived burden related to data overload, and managing expectations, she said.
5) Use a systematic approach for data interpretation. The Panther Program website offers separate pages for the Dexcom and Libre CGMs, and the commercial AID systems Control-IQ, Omnipod 5, and Minimed 780G.
For each, the approach to data interpretations involves three steps: A “big picture” analysis examining CGM use, glycemic metrics (ie, time in range), and glucose patterns of highs and lows, followed by a “small picture” dive using weekly reports to identify the causes for the glycemic patterns, and then devising a plan to help patients learn from the patterns to insulin pump settings.
Everything on the Panther website is free, Berget said.
‘Maintain Your Mental Time in Range’
Edelman, who is founder and director of the “nonprofit diabetes edutainment organization” Take Control of Your Diabetes, offered several additional pointers regarding CGM use. He said that CGM is “the most important advance for people with type 1 diabetes since the discovery of insulin.” He also pointed out that prior to CGM, it was virtually impossible for people with type 1 diabetes to stay in target glucose range.
And even with the technology, he noted, “The reality is people bounce around. They go low, they go high. I think it’s nice to acknowledge that they don’t have to be perfect all the time.”
Regarding CGM use, Edelman also advised:
Educate your patients to respond to trend arrows. While most automated systems account for the arrows indicating that blood glucose rising or falling, it’s important for patients to understand how to adjust their insulin doses as well, Edelman said, noting that most providers don’t do this.
Basically, patients need to understand that when the arrow goes up, they need more insulin. But when the arrow goes down, they may need nothing and should wait until they stabilize, he said.
Set alerts and alarms. “Alerts and alarms are your friends,” Edelman said. Changing the alarm settings can help improve time in range without changing the insulin delivery settings, just by lowering the upper alarm alert during the day from the default 180 mg/dL to 150-160 mg/dL, while keeping it set higher at night to avoid alarm fatigue.
Strongly encourage learning about a hybrid closed-loop system. “I ask my patients to look at each one carefully before deciding. I hook them up with the sales representatives and tell them not to make a decision until they’ve seen them all. Then we have a conversation. The one they pick is usually the one that’s going to be successful. And of course, there is also the [do it yourself] looping option.”
Edelman also provided other tips for managing common type 1 diabetes challenges, including reducing post-meal glucose spikes by bolusing at least 20-30 minutes prior to eating or using the fast-acting inhaled insulin Afrezza and reducing — although not necessarily eliminating — carbohydrate consumption, a practice he called “going low carb-ish.”
He also advised cautioning patients about over-treating low blood glucose, always keeping an unexpired and easily administered glucagon preparation on hand, and using exercise to reduce high blood glucose.
Importantly, he concluded, “Maintain your mental time in range. You are your own best advocate. Be smart and be persistent. Knowledge is power. Celebrate the victories, no matter how small they seem.”
Berget is a consultant and/or speaker for Insulet, Medtronic, Tandem, Dexcom, and Embecta. The PANTHER program received support from Insulet and Tandem. Edelman serves on the board of directors for Senseonics.
Miriam E. Tucker is a freelance journalist based in the Washington, DC, area. She is a regular contributor to Medscape, with other work appearing in the Washington Post, NPR’s Shots blog, and Diatribe. She is on X: @MiriamETucker.
